4 Apr 2016
Management of traumatic and surgical wounds in cats and dogs
Daniela Murgia offers advice for treating and managing skin tissue injuries, including antimicrobial treatment, preventing contamination, suitable dressings and healing options.

Figure 1b. The same Labrador retriever with a degloving injury of the right medial tarsus.
Managing traumatic and surgical wounds is a frequent event in small animal veterinary first opinion practice.
The decision when to close a wound and how, or continue to treat it as open, is a key question and depends on several factors that should be revisited during the course of wound management.
Factors to consider include:
- time since occurrence
- extent of tissue trauma
- amount of local tissue loss
- degree of bacterial and foreign body contamination
- patient’s overall condition
- degree of tissue ischaemia and local blood supply
- possibility of closure based on wound location
- possibility of closure without tension or unacceptable dead space
- likelihood of complications, such as contracture or wound dehiscence

Species differences must be considered when planning wound management. For example, open wounds heal slower in cats compared with dogs.
Patients with non-healing, or delayed healing, of open wounds should be evaluated for conditions that may interfere with the process. Delay factors include local ischaemia, multi-resistant bacterial contamination, necrotic tissue and tension.
Systemic disease such as diabetes mellitus, hypothyroidism, or hyperadrenocorticism, and malnutrition with hypoproteinaemia or vitamin deficiencies, can also interfere with the healing process.
Initial assessment
Animals with traumatic wounds should be assessed for any further life-threatening injuries. The cardiorespiratory system should be functional, with consideration given to thorax radiography and abdominal cavity ultrasonography.
Pain management is mandatory in traumatised patients. Opioids, such as methadone, and NSAIDs are valuable choices. NSAIDs should not be administered in hypovolaemic patients due to the possible renal and gastrointestinal side effects. Local analgesia using lidocaine or bupivacaine provides good local pain control with reduced systemic effects.
Traumatised patients should be monitored and reassessed regularly as they may destabilise rapidly (Figure 1).
Antimicrobial treatment and antibiotics
Bacterial infection can delay wound healing, so topical products are indicated early in wound management to reduce bacterial contamination.
Topical agents cover a broad bacterial spectrum and include antimicrobial/silver-based ointments (silver sulfadiazine), silver-based dressings and hyperosmotic substances such as sugar, honey and 20% hypertonic saline.
Honey
Honey is a natural product and its effectiveness may vary with the source of the product and the processing methods used – its medical use is, therefore, recommended.
Honey is available as raw honey in tubes or jars, or impregnated dressings. Its osmotic effect dehydrates microorganisms, reducing oedema and inflammation, and promoting granulation tissue formation and epithelialisation.
Honey can be used in the inflammatory and early repair phases of healing, and stopped when debridement is complete and healthy granulation tissue is present.
A honey-soaked gauze dressing may need replacing one to three times daily in highly exudative wounds, or once every one to three days if the wound produces a small amount of exudate. The gauze may adhere to viable tissues causing pain on removal. This can be avoided using a hydrophilic dressing impregnated with honey.
Sugar
Sugar has hypertonic effects similar to honey and enhances granulation tissue formation and epithelialisation, but does not have the same anti-inflammatory and wound stimulation effects.
Sugar is applied in a 1cm thick layer on the wound and covered by an absorbent bandage. Bandage changes are required two to three times daily to maintain the osmolality of the wound.
Diagnosis
Wound infection diagnosis should be based on culture and sensitivity of samples taken from the deep wound tissue. These results should inform selection of systemic antibiotics.
Acute wound infections are usually characterised by the presence of one dominating microorganism, while chronic infections are often polymicrobic and possibly multi-resistant. Systemic antimicrobial therapy is indicated for progressing cutaneous infections or infections involving the deeper tissues.
Antimicrobial treatment can be stopped once healthy granulation tissue has formed because penetration into granulation tissue is limited.
Only wounds with localised signs of infection may be treated by topical methods alone.
Initial wound care

Contaminated wounds should be managed as open wounds until they can be closed or heal by second intention. Immediate wound management is aimed at reducing the bacterial burden and preventing further contamination.
Irrigation has an important role as it allows removal of the gross contamination (bacteria, foreign material and necrotic debris). The sterility of the solution and any antimicrobial properties are not as important as its availability in copious volumes.
Clinical studies evaluating tap water and sterile saline for wound irrigation in humans showed no difference in occurrence of wound infection (Whaley, 2004).
Despite its hypotonic nature, which can cause cellular destruction, tap water is acceptable for the initial irrigation. Valid alternatives for wound irrigation are:
- balanced electrolyte solutions (lactated Ringer’s, Hartmann’s)
- unbalanced electrolyte solution (0.9% saline)
- antiseptic irrigation solutions:
- – 0.05% chlorhexidine solution using 10ml of chlorhexidine gluconate (5% concentrate) added to 500ml sterile water
- – 0.1% povidone iodine solution using 50ml of povidone iodine (10%) added to 500ml balanced electrolyte solution
The ideal amount of pressure used to flush wounds has not been established. Very high pressure, such as that produced by pulsatile lavage instruments, may drive contaminants and debris into deeper tissue planes and damage the tissue, which could reduce the resistance to infection.
A common technique is to use a 35ml syringe with an 18-gauge needle to generate 7psi to 8psi of pressure. Low-pressure irrigation can also be used by flowing fluid from a given set connected to a bag of sterile solution, or pouring fluid from a sterile bottle, or by using a bulb syringe.

Initial wound care should also include covering the wound with a clean, dry bandage to prevent further contamination and haemorrhage, and to stabilise the injured area. The covering remains in place until definitive treatment can be performed. In areas where the bandage may be difficult to place, the dressing can be secured with a tie-over technique (Figure 2).
Thorough wound assessment and definitive wound management will require sedation and general anaesthesia, which should be delayed until the animal has been stabilised.
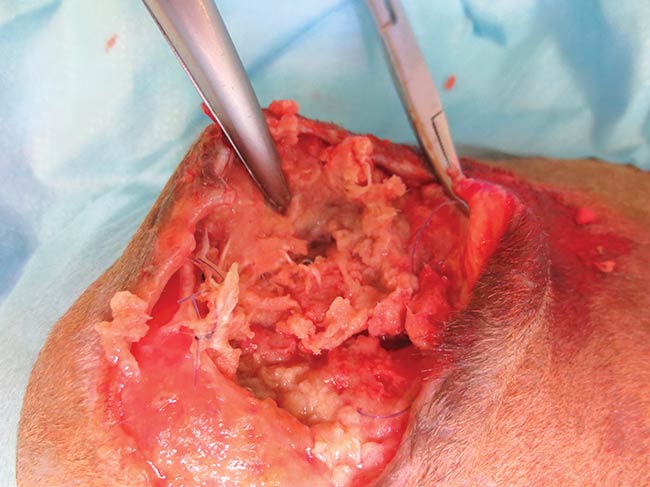
Debridement
Wound debridement is indicated to remove foreign material and devitalised or necrotic tissue. It may be selective or nonselective.
Selective debridement involves using enzymes to remove only damaged tissue, leaving the healthy tissue in place. Nonselective debridement involves physical removal of debris, including some healthy tissue. The previously mentioned wound irrigation is a nonselective debridement technique.
Sterile instrumentation and aseptic technique should be used for surgical debridement. Foreign debris not removed by wound irrigation can be removed with thumb forceps, scalpel blade and curette. However, excessive excision of healthy tissue could delay wound healing. The aim of debridement is to have a well-vascularised wound bed to support healing.
Tissue viability can be difficult to assess, so initial tissue debridement should be conservative. In fact, skin circulation may deteriorate for five days after trauma or surgery because of oedema and other factors, so repeated debridement may be required as the extent of tissue necrosis becomes more evident.
Skin viability is clinically assessed by colour, warmth, pain sensation and bleeding. Non-viable necrotic skin is black or white and may be non-pliable, cool and devoid of sensation; normal skin is warm, pliable and pink with pain sensation, while questionable areas are blue or purple and sensation is poor.
Layered debridement describes sequential removal of devitalised tissue at the wound’s surface, progressing to the wound depth. Exposed cortical bone, fat and fascia are not well-vascularised tissues.
Forage of exposed cortical bone (penetration of the bone in multiple sites with a pin creating multiple holes) allows the vascular medullary canal to communicate with the wound bed, inducing formation of granulation tissue. Excess fat should be removed and intact fascia opened to expose underlying vascular muscle tissue.
Enzymatic debridement and autolytic debridement are further forms of selective debridement.
Enzymatic debridement uses agents applied to the wound surface to selectively destroy necrotic tissue and bacterial biofilm. This technique can be used instead of surgical debridement in patients with anaesthetic risk, or with other surgical contraindications. Enzymatic agents are available as ointments or gels containing streptokinase, trypsin, proteinase and collagenase. Enzymatic debridement occurs without pain or bleeding, can be slow and expansive and is not indicated to treat large areas.
Autolytic debridement occurs when a moist environment is maintained at the wound surface. The moisture allows normal cellular processes to destroy bacteria and remove or repair damaged tissue. Autolytic debridement is promoted by using hydrophilic, occlusive or semi-occlusive bandages that allow some wound exudate to remain in contact with the wound surface and keep it moist.
Wound exudate contains endogenous enzymes and growth factors that stimulate angiogenesis, granulation tissue formation and epithelialisation.
Bandages also keep the wound surface warm, which enhances enzymatic activity. Proper wound preparation is needed to create an optimal environment for autolytic debridement.
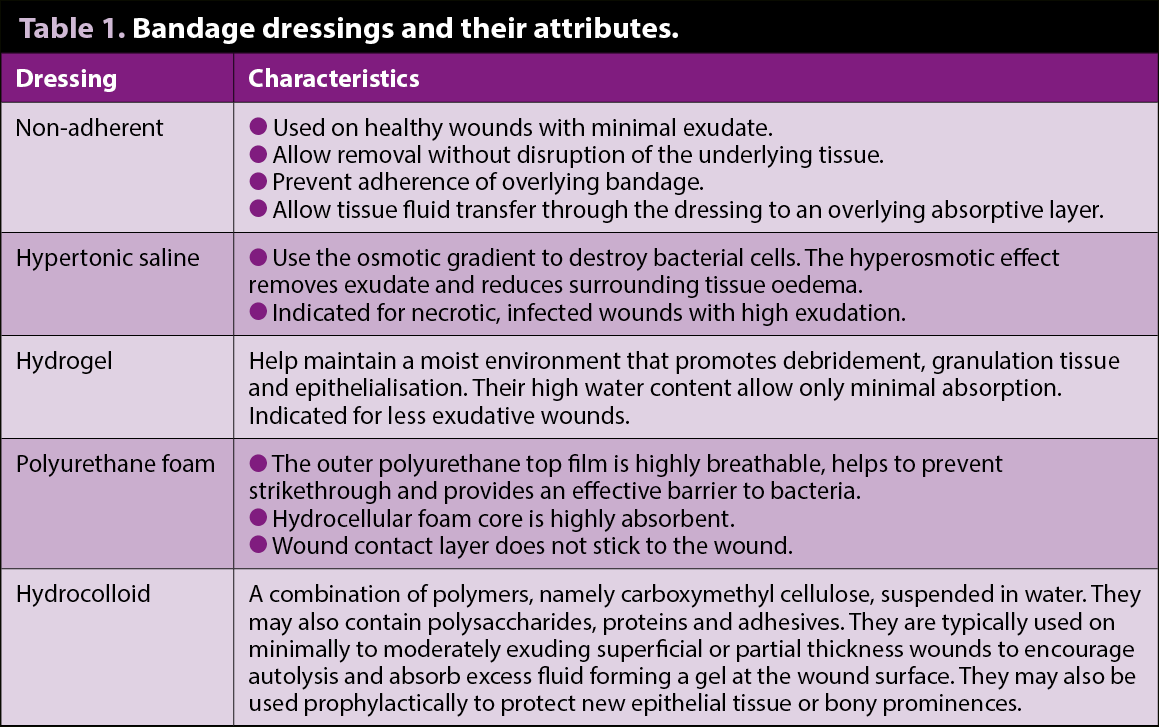
The principle of moist wound healing is put into practice by the use of hydrophilic dressings (Table 1).
Wound closure
There are four healing options:
- first intention healing (primary wound closure)
- delayed primary closure
- second intention healing (healing by contraction and epithelialisation)
- third intention healing (secondary closure)
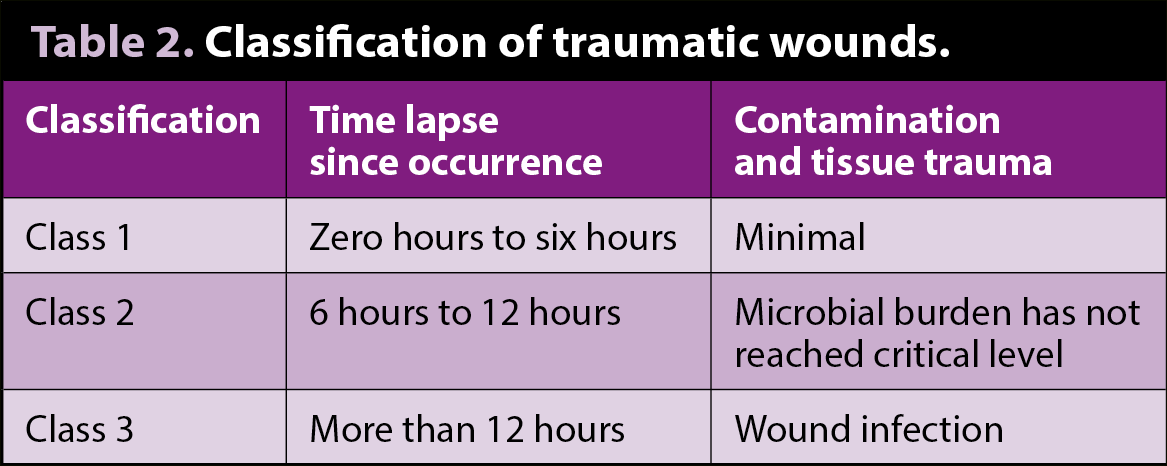
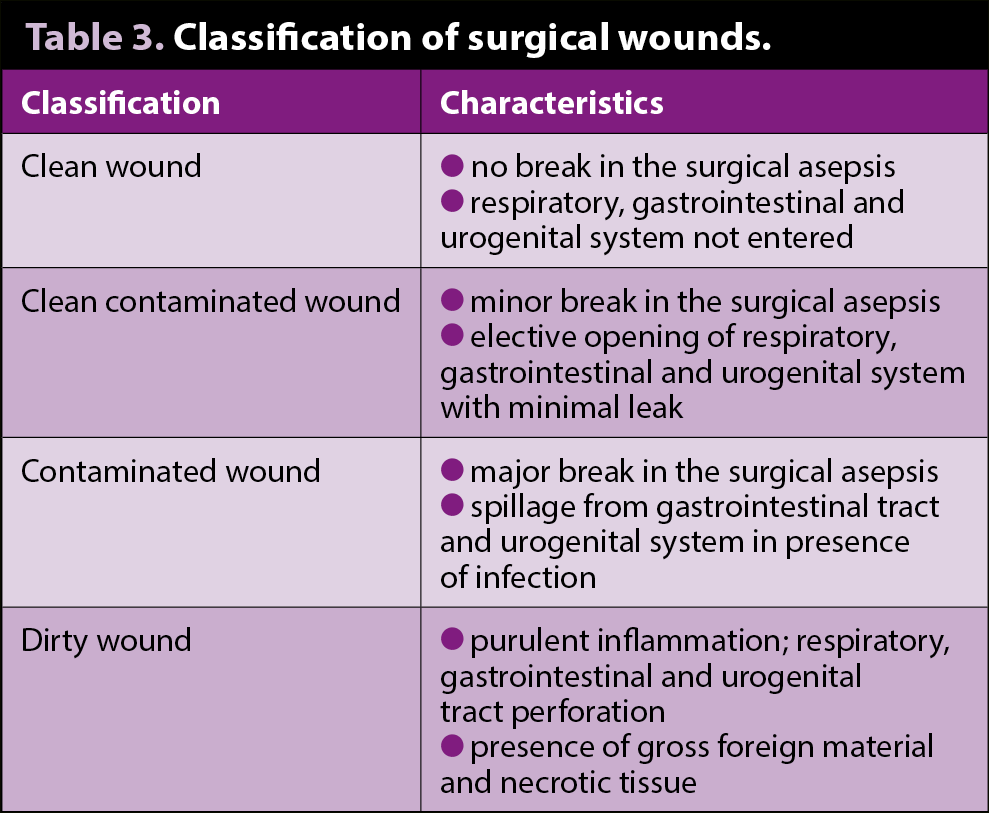
First intention healing consists of apposing the wound edges with sutures, staples or glue. It occurs in surgical wounds and is indicated in clean or minimal contaminated wounds. Class 1 wounds (Table 2) can be closed with primary wound closure.
Delayed primary closure consists of apposing the wound edges three to five days after wounding, before granulation tissue has been formed. Class 2 wounds or mildly contaminated wounds (Tables 2 and 3), requiring some debridement and open wound management, can be managed with delayed primary closure.
Second intention healing occurs when the wound is left open, allowing formation of granulation tissue until wound closure happens by contraction and epithelialisation. This healing is indicated for dirty wounds (Table 3) in which debridement and cleansing is necessary, but primary or delayed closure is not permitted.
Third intention healing occurs when appositional wound closure happens three to five days after wounding following formation of granulation tissue.
In the author’s experience, each wound is different so it is difficult to give a precise rule about timing of wound closure. Contaminated wounds should never be closed primarily and should be revisited during the course of the management to choose the most appropriate timing and closure option.
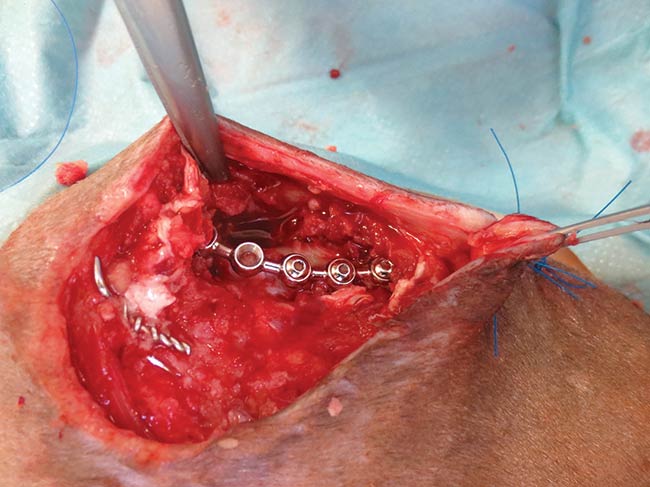
Some patients require wound care for several days before the wound environment is suitable for closure. Vacuum-assisted closure (negative pressure wound therapy; NPWT) improves the wound environment and speeds up wound healing. NPWT involves the use of topical negative pressure, or suction, applied to an open wound that has been covered with porous foam and then covered by an adherent, occlusive sheet to achieve an airtight seal (Figure 3).
Applied controlled negative pressure (subatmospheric; -80mmHg to -120mmHg) pulls exudates through the foam into a reservoir, resulting in active drainage and decreased oedema. Negative pressure increases blood perfusion and neoangiogenesis to the wounded tissue, allowing delivery of oxygen, nutrients, cells (fibroblasts) and growth factors. Increased blood perfusion also removes free radicals and waste products and, for patients receiving antibiotics, increases the delivery of antimicrobials to the wound.
Reduced bacterial burden in the wound has been proposed as a mechanism that leads to improved wound healing with NPWT.
Indications for NPWT include chronic non-healing wounds, infected wounds, dehisced wounds, ulcers, skin grafts and skin flaps. NPWT should not be used in the presence of any local malignancy, because of the risk of local tumour recurrence. It should not be used over exposed vessels, tendons, ligaments and nerves because damage could occur; severe haemorrhage could result if NPWT is placed over arteries or veins.
The NPWT system needs to be monitored at least every two hours for any evidence of suction loss.
The character and volume of the fluid from the wound also needs to be monitored to determine the effectiveness of NPWT in controlling infection and to verify drainage volume is declining. The canister needs to be emptied or changed when it approaches its maximum capacity.
Dressings can be left in place for up to three days before changing, though loss of suction and loss of the airtight seal require anticipation of the dressing change.
NPWT seems to offer great benefit for the patient in terms of faster wound healing, such as quicker and improved vascularity, decreased oedema, increased granulation tissue formation, increased wound contraction and potentially decreased bacterial contamination.
Conclusion
The goal of open wound management is to limit any further contamination and maintain the wound moisture for infection control and faster wound healing.
Dressing selection changes with the progress of the wound healing and amount of exudate.
Managing chronic non-healing wounds can be more complex and may require advanced adjunctive therapies, such as NPWT.
- Some drugs mentioned are used under the cascade.