26 Sept 2023
Abnormalities and injuries of the lumbosacral spine in cats
Philip Witte discusses spinal trauma, which occurs more in feline patients than in canine patients, as well as possible treatments.

Image © Krakenimages / Adobe Stock
Cats present less frequently than dogs, with signs consistent with hindlimb lower motor neuron disease. We see cats affected by congenital deformities, which are commonly mistaken for traumatic injuries, but we also see traumatic injuries to the spine in cats – in particular resulting from road traffic collisions.
The most common spinal trauma in cats is sacrocaudal luxation (tail pull injury), which is discussed in this article, as an understanding of this condition’s influence on bladder function aids an understanding of other caudal vertebral disease.
Sacral injuries are also more frequent in cats than in dogs – typically associated with pelvic fractures. This article will focus on injuries and abnormalities of the lumbosacral spine. It will focus on three specific abnormalities: fracture/luxation of the L7-S1 intervertebral space, lumbosacral transitional vertebrae, and degenerative lumbosacral stenosis to highlight the importance of this anatomical region, as well as suggested routes for investigation and treatment.
Neuroanatomical localisation
Focal lesions of the spine are more common in cats than in dogs (in which more diffuse myelopathies are somewhat more frequent), so attempts should always be made to neurolocalise the site of the lesion. When dealing with neurological disease in dogs or cats, neurolocalisation involves an assessment of nerve function, which often frightens the clinician, but can be remarkably simple (Table 1).
| Table 1. A guide to neurolocalisation of focal myelopathy | |||
|---|---|---|---|
| Lesion location | Forelimb | Hindlimb | Bladder, anus, tail |
| C1-C5 | UMN | UMN | UMN |
| C6-T | LMN | UMN | UMN |
| T3-L3 | Normal | UMN | UMN |
| L4-S3 | Normal | LMN | LMN |
| S1-S3 | Normal | Normal | LMN |
| UMN = upper motor neurone (that is, the limb is weak, but myotatic reflexes are intact), LMN = lower motor neurone (that is, the limb is weak and myotatic reflexes are reduced or absent). |
|||
For the purposes of this article, the emphasis will be on cats in which forelimb function is normal, hindlimb function is abnormal, and bladder/anus and tail function are also abnormal. Distinguishing between neurolocalisation to T3-L3 and L4-S3 relies on the presence or reduction of the hindlimb myotatic reflexes (patellar reflex and flexor/withdrawal reflex). The patellar reflex is assessed through percussion with a reflex hammer.
The flexor/withdrawal reflex involves pinching the interdigital skin on the hindlimb in question and monitoring for withdrawal of the limb.
Note that flexion of all joints in the limb is the positive response, and this is not an assessment of nociception (the conscious perception of noxious stimuli). In other words, despite complete severance of the spinal cord at the level of the T3-L3 segments, the hindlimb flexor/withdrawal reflex can still be functional; however, no nociception will occur (that is, the cat will not be consciously aware of the stimulus and will, therefore, not turn to look, scratch the operator or attempt to move away from the stimulus).
The spinal cord in a cat terminates at the level of the L6 vertebral body. As such, the L5 spinal cord segment (from which the L5 nerve roots derive) is located over the L4-L5 intervertebral disc space; the L6, L7 and S1 segments are dorsal to the L5 vertebral body; and segments S2 and S3 are dorsal to the L6 vertebral body.
Caudal to the level of the L6-L7 intervertebral disc space, the spinal cord is no longer present and nervous tissue in the vertebral canal exists as the cauda equina – essentially, the peripheral nerves of the L7, sacral and caudal segments.
How is sacrocaudal luxation relevant in a discussion of lumbosacral injuries?
The pelvic nerve consists of contributions from the nerve roots of S1, S2 and S3. It supplies sensory and motor innervation to the bladder, descending colon and rectum.
The pudendal nerve also consists of contributions from the nerve roots of S1, S2 and S3. This nerve provides sensory information from the urethra, anal sphincter and perineum, and motor innervation to the urethra and anus.
A tail pull injury theoretically results in traction on the S1-S3 nerves, sparing hindlimb function, but resulting in variable disruption of conscious urinary bladder function. Unfortunately, while theoretically this should typically involve a lower motor neuron bladder (flaccid and easy to express), various reasons exist (resentment in particular) that manual expression may still be difficult, potentially necessitating bladder management involving indwelling urethral catheterisation.
A return of bladder function may be expected within a few days. If no return of bladder function has occurred by two weeks, the prognosis is poor. If no return of bladder function has occurred by four weeks, the prognosis is grave.
The relevance to lumbosacral injuries is that similar bladder/anus and perineum signs may be observed in cats with lumbosacral lesions, since the S1, S2 and S3 nerve roots pass dorsal to the L7-S1 intervertebral disc space. Therefore, signs and management are similar, and a similar conversation with the clients regarding prognosis should be had.
Lumbosacral fracture/luxation
Fractures and dislocations of the feline caudal lumbar spine are often severely displaced in cats, and typically follow high-impact trauma. Despite rather severely displaced lumbosacral fracture/luxation, cats can often show surprisingly good nerve function (hindlimb motor function or good sensation, perineal tone, tail motor function and so on) indicating that nerve roots are intact and not completely severed, such that the prognosis for return of function is not necessarily grave.
When assessing spinal stability with respect to whether surgical stabilisation is indicated, we divide the vertebral column into three compartments:
- The dorsal compartment (lamina and pedicles, articular processes, and the associated ligamentous and joint capsule structures).
- The middle compartment (dorsal portion of the vertebral body, dorsal longitudinal ligament and dorsal aspect of the annulus fibrosus).
- The ventral compartment (ventral portion of vertebral body, ventral longitudinal ligament and ventral aspect of the annulus fibrosus).
Where two or more compartments are traumatised then surgical stabilisation is recommended.
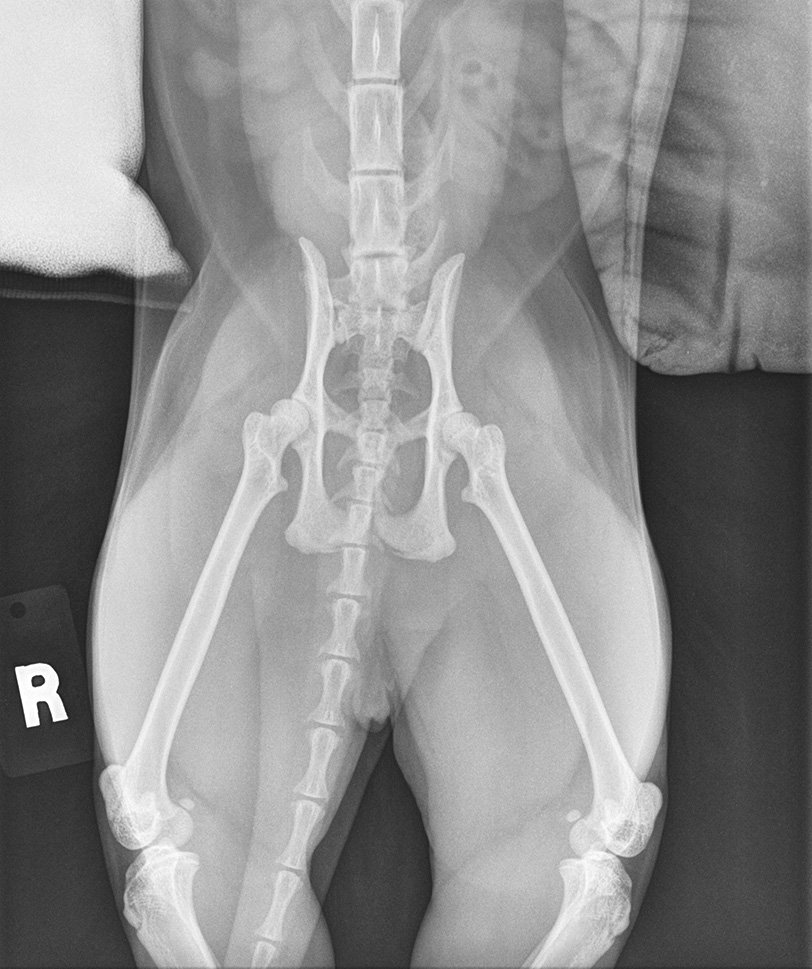
Figure 1 shows mediolateral and dorsoventral projections of the pelvis and surrounding structures of a one-year-old female, neutered domestic shorthair presenting with reluctance to bear weight on the hindlimbs, paraparesis and resentment to palpation in the region of the pelvis.
Examination revealed normal forelimb function with moderate paraparesis (weakness in the hindlimbs). Proprioception could not be assessed as the cat was reluctant to stand. The patellar and hindlimb withdrawal reflexes were reduced. A large bladder was present, which was difficult to express. Anal tone was present, but reduced. Tail motor function was present, but weak.
Neurolocalisation was to the L4-S3 spinal segments. The images reveal deviation of the spine at the level of the lumbosacral junction in the dorsoventral view. A fracture of the caudal end plate of the L7 vertebral body is present.
Despite relatively minimal displacement, the imaging suggests trauma to the ventral and middle compartments of the vertebral column at that level, indicating surgical stabilisation. Close scrutiny of the images also reveals a suspicion of trauma to the caudal end plate of the S3 vertebral body, suggesting a possible additional sacrocaudal luxation-type injury. The relative contributions to reduced perineal, anal, and urethra motor and sensory function from these two injuries (L7-S1 fracture/luxation and S3-Ca1 fracture/luxation) are not possible to determine. However, surgery to address the lumbosacral dislocation is indicated to prevent further injury to the nerves within this unstable unit and improve comfort.
Fixation to stabilise the fracture itself is not possible as the small size of the end plate fragment precludes implant placement. Therefore, the L7-S1 unit is stabilised through bridging fixation.
Vertebral fracture fixation and stabilisation of two or more vertebrae requires implant placement into the vertebral body. Fixation of the dorsal lamina, pedicles or dorsal/lateral processes is typically considered insufficient since these narrow processes of bone lack sufficient stiffness.
Fixation is usually performed through a ventral approach in the cervical spine, applying ventral fixation and a lateral (or dorsolateral) approach in the majority of the thoracic and lumbar spine, with lateral fixation.
In the lumbosacral spine, the preferred approach is through a dorsal midline incision and application of plates from dorsal. Screws are directed into the L7 vertebra through the pedicles and into the vertebral body in a dorsoventral direction, and into the sacral wings to diverge in a direction parallel with the sacroiliac joints to maximise bone purchase.
Fixation can involve threaded pins driven into the bones and linked to one another using epoxy putty or plates and screws. Where plates are applied, the irregular contour of the dorsal aspect of L7 and the sacrum make accurate contouring of a plate essentially impossible. Therefore, application of conventional plates and screws is not possible. In this case, two parallel 2mm String of Pearls plates were applied with 2mm screws (Figure 2).
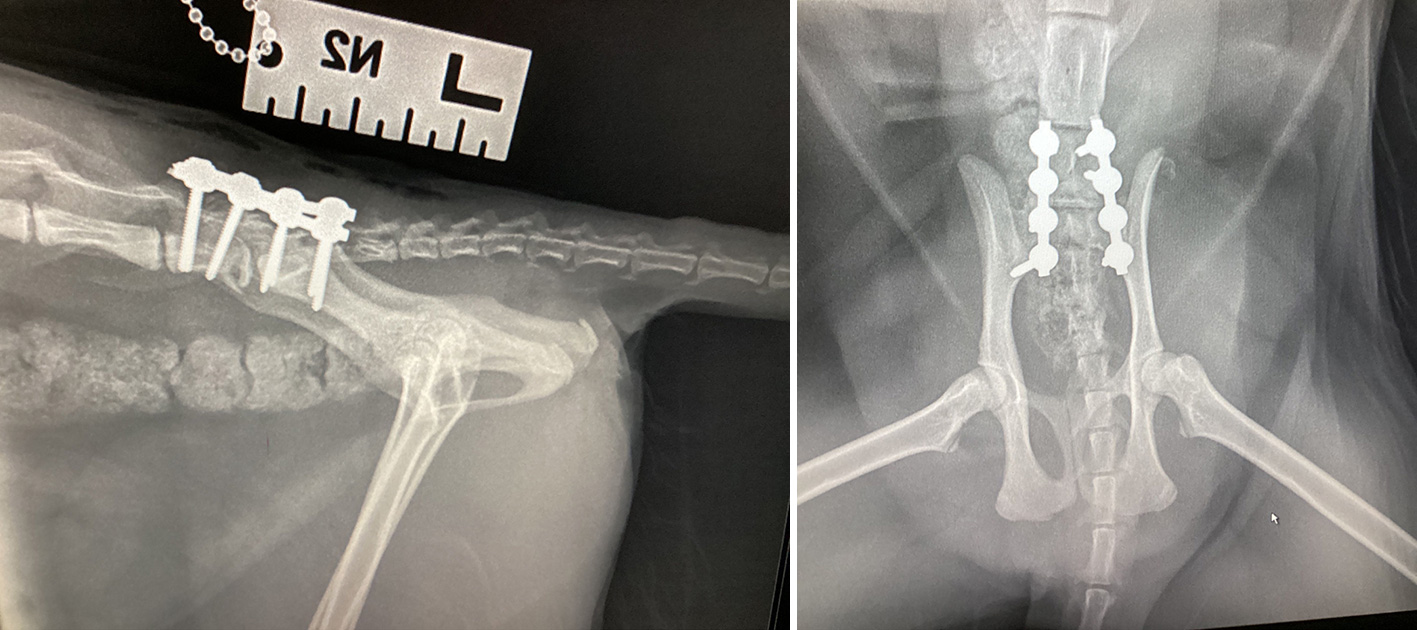
The outcome for this cat was excellent. Mild deterioration occurred in terms of tail motor function and hindlimb motor function during the 24 hours following surgery. Manual bladder expression was required for three days following surgery, after which hindlimb motor function, tail motor function and urinary bladder function demonstrated sufficient improvement for discharge to the care of the owners.
Postoperative management involved three weeks of confinement to a crate with short periods of controlled activity in a single room frequently through the day, three weeks of confinement to a single room and four weeks of confinement to the house prior to reintroduction of outdoor exercise.
Hindlimb motor function appeared to return to normal, with the cat returning to climbing and jumping as prior to the injury.
Lumbosacral transitional vertebrae
Congenital deformities of the spine are relatively uncommon in cats. Lumbosacral transitional vertebra refers to a few congenital conditions in which the final lumbar vertebra (which may be extra) demonstrates sacral anatomical characteristics.
Transitional vertebrae may demonstrate asymmetry, with the transverse processes typically used to classify the nature of the deformity, that is, for each side of the transitional vertebra the transverse process is classified as:
- Lumbar – narrow, cranially deviated and not in contact with the ilium.
- Intermediate – lumbar in nature, but contacting or superimposed on the ilium in a dorsoventral radiographic projection.
- Sacral – demonstrating the characteristics of a sacral wing.
In terms of clinical signs, an asymmetrical transitional sacral segment can result in rotation of the pelvis about its long axis. In dogs, this is reported to be most severe in cases with asymmetrical transitional sacral vertebrae in which there is no intermediate transverse process (that is, sacral on one side and lumbar on the contralateral side).
Rotation of the pelvis can influence dorsal acetabular coverage of the femoral head on one side, resulting in unilateral signs of hip discomfort and OA.
In addition, the clinical signs may be associated with nerve root impingement either as a result of abnormally shaped foramina or through soft tissue hypertrophy secondary to forces through the abnormal intervertebral junction.
The majority of cats demonstrate no clinical signs at all in association with their lumbosacral transitional vertebrae. Clinical signs can vary from significant resentment to palpation in the region of the lumbosacral spine – presumably in association with foraminal stenosis/nerve root impingement to hindlimb lameness associated with hip OA.
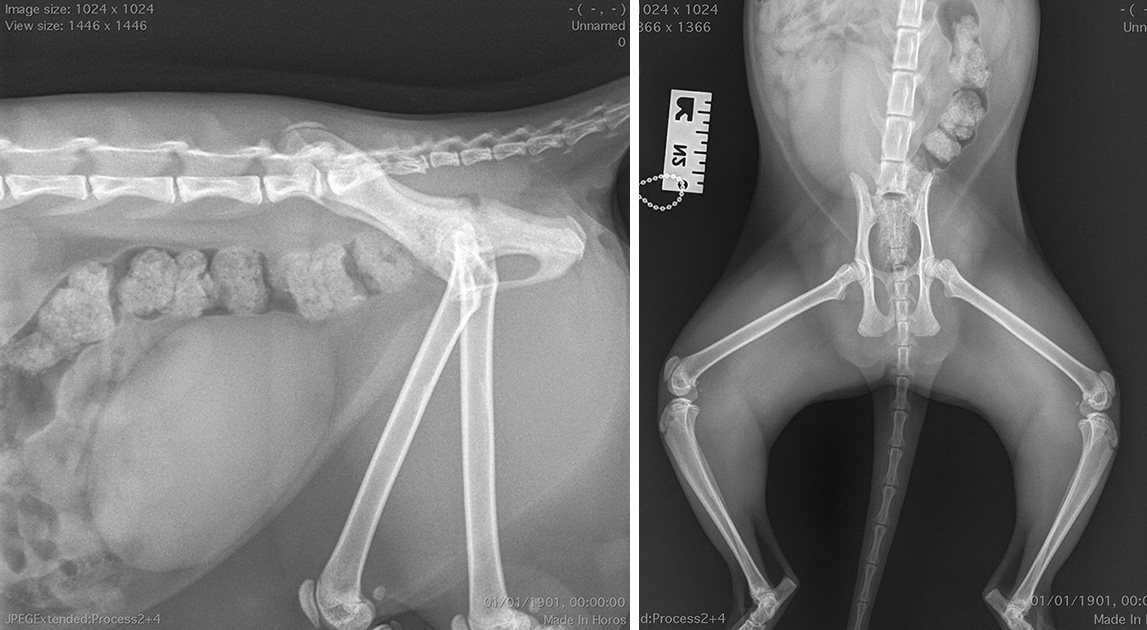
Some cats present very young, while others present later in life. Plain radiography is used to confirm the diagnosis and investigate the severity of deformity in the lumbosacral spine. Figure 3 shows the radiographs of three cats with transitional sacral segments. Their presenting signs and management protocols (and plans) are given.
In cases where treatment with conservative management alone is unsuccessful, a need exists to determine for sure which component of the disease is the cause of the signs. Where significant hip OA is present, hip salvage (total hip replacement or femoral head and neck ostectomy) may be indicated.
However, the majority of cases in which conservative management is not successful will involve nerve root impingement and further investigations and treatment may be as for degenerative lumbosacral stenosis (see further on).
Degenerative lumbosacral stenosis
The majority of our understanding of degenerative lumbosacral stenosis comes from the literature regarding this condition in large-breed dogs, in which it is reasonably common. There is narrowing of the vertebral canal and/or foramina at the level of the lumbosacral junction. Narrowing can be from any direction, with L7-S1 disc protrusion, hypertrophy of adjacent soft tissues (ligamentous and synovial structures), osteophyte formation on the articular facet joints, spondylosis deformans extending from its typical ventral position to the foramina and spondylolisthesis (cranioventral tipping of S1 relative to L7).
Degenerative lumbosacral stenosis is a disease of older cats. The signs typically include a chronic and progressive deterioration in hindlimb function, with avoidance of jumping, hindlimb lameness, a low tail carriage and defecation outside the litter tray being frequently reported.
Clinical signs of nerve root +/− cauda equina compression in degenerative lumbosacral stenosis include hindlimb neurological deficits. As a result of the location, the signs should be lower motor neuron in nature – that is, the myotatic and flexor/withdrawal reflexes should be reduced. The sciatic nerve, arising significantly from the L7 nerve root, is often most affected (hock flexion may be weak such that the digits are scuffed on the ground during walking).
Investigation involves plain radiography, which may show narrowing of the L7-S1 intervertebral disc space, end plate sclerosis, spondylosis deformans and spondylolisthesis. See Figure 4 for a case demonstrating all these features of degenerative lumbosacral stenosis.

Treatment options for degenerative lumbosacral stenosis include conservative management (analgesia including NSAIDs and gabapentin, body condition optimisation and lifestyle changes) or surgery. Reported surgical options include dorsal laminectomy to decompress the nerve roots and stabilisation of the lumbosacral junction (with or without decompression).
Where stabilisation is performed without specific decompressive surgery, decompression may occur through restoration of more normal alignment during surgery (reduction of spondylolisthesis should increase the diameter of the foramina) and through atrophy of soft tissue structures, which are no longer under strain.
Decompression by foraminotomy alone, as is frequently reported in dogs, has not as yet been reported in cats. Long-term outcomes for decompression and stabilisation have been reported to be subjectively good.
Conclusion
Signs consistent with traumatic, congenital or degenerative disease of the lumbosacral spine are not rare in cats. Through thorough examination and in-house imaging, a lot can be done by the general practitioner to diagnose conditions including lumbosacral fracture/luxation, lumbosacral transitional vertebra and degenerative lumbosacral stenosis.
Treatment of all three conditions can offer a very good prognosis, although three-dimensional imaging and relatively advanced surgery may be indicated in some cases.
Latest news

Small animal
Evidence-based clinical nutrition to support weight management and joint care in dogs
Sponsored
28 Feb 2025