30 Sept 2019
Fungal osteomyelitis in a dog
Selda Curtseit presents the case of Ella, a nine-year-old neutered female Rottweiler with a history of OA, in the latest of the occasional Case Notes series.

On examination, she elicited pain at palpation of the forelimb joints; a firm swelling on the right second metacarpal was also present (Figure 1).
Rectal temperature, heart and respiratory rates were within normal limits. Blood work showed mild monocytosis (1.96 × 109/L; reference range 0.16 × 109/L to 1.12 × 109/L), mild increase of alkaline phosphatase (ALP; 290U/L; reference range 23U/L to 212U/L) and hyperglobulinaemia (49g/L; reference range 25g/L to 45g/L).
Initially, she was treated with firocoxib, diazepam and buprenorphine. Two days later, the spinal pain had significantly improved, but Ella still showed 5/10 lameness on her right foreleg.
Radiographs taken under sedation showed no evidence of spinal lesions. Both carpi appeared thickened medially, with reduced capacity for flexion. The grossly swollen right second metacarpal showed a mixed osteolytic and osteoproliferative lesion (Figure 2).
Given Ella’s age and breed, a bone tumour (for example, osteosarcoma) was suspected. Chest radiographs were unremarkable.
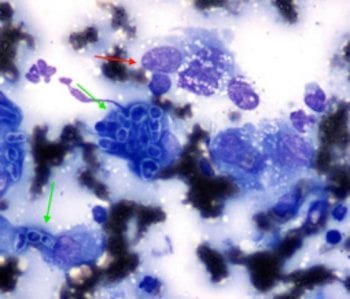
A fine needle aspirate was taken from the bone swelling and submitted for cytology. A diagnosis of fungal osteomyelitis was made, based on the presence of fungal hyphae in the aspirate admixed with inflammatory cells, mostly macrophages (Figure 3).
A second aspirate was taken for fungal culture and Aspergillus terreus was identified. An antifungal susceptibility test was performed by disc diffusion method, and sensitivity for itraconazole, voriconazole and amphotericin B recorded.
Answer
Aspergillus is a fungus that is ubiquitous in the environment and an opportunistic pathogen.
Of the two common canine infections caused by Aspergillus species – nasal and disseminated aspergillosis – the latter is the less frequently encountered. The two types of infections do not appear to be related, but a report of a dog that developed fungal osteomyelitis six months after treatment of nasal aspergillosis raises this possibility.
Aspergillus fumigatus is the most common pathogenic species and A terreus is the most common species associated with disseminated aspergillosis.
German shepherd dogs appear predisposed to disseminated disease; however, immunosuppression caused by long-term treatment with ciclosporin and corticosteroids may increase the potential for infection in any breed.
The portal of entry usually remains unknown, although entry through the respiratory or gastrointestinal tract is most likely, with subsequent haematogenous dissemination. Disseminated aspergillosis may also result from entry following surgery or IV inoculation.
In general, canine aspergillosis carries a poor prognosis, with most cases of disseminated aspergillosis euthanised. Several studies described attempts to treat disseminated aspergillosis using fungicidal drugs, fungistatic medications or newer classes of antifungal medications, including echinocandins and terbinafine.
Using these drugs alone or in combination, infection was eliminated in only one case, while euthanasia was elected within a year in most cases due to progression of disease. Nevertheless, itraconazole is considered the most effective drug and has fewer side effects.
Long-term clinical remission achieved with itraconazole alone was described in a case of disseminated aspergillosis (for 2.7 years) and a case of non-disseminated Aspergillus discospondylitis (for 8 years), respectively.
Haematology and biochemistry in aspergillosis ranges from unremarkable to showing neutrophilic leukocytosis, monocytosis and increased globulins, reflecting chronic inflammation. In Ella’s case, mild increase of ALP was also noted and likely associated with osteolysis, due to increased osteoblastic activity.
Ella was started on oral itraconazole at 4.7mg/kg every 24 hours, alongside one-and-a-half tablets containing codeine phosphate and paracetamol, and 600mg gabapentin. In the following four weeks, the lesion became increasingly painful and a clinical suspicion of a pathological fracture arose.
The decision was made to amputate the affected bone and oral itraconazole was continued for a further two weeks post-surgery.
Some drugs are used under the cascade.


