19 Mar 2018
Gall bladder mucocele in a dog
A look at the case of Smartie, an 11-year-old female neutered border terrier presenting with a 36-hour history of lethargy and vomiting.

Your final case of the morning is Smartie, an 11-year-old female neutered border terrier. Smartie has been presented to you for investigation of a 36-hour history of lethargy and vomiting.
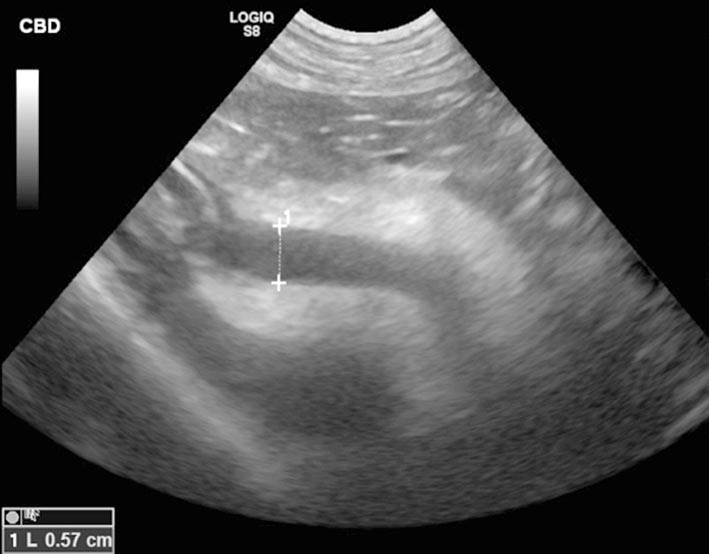
Biochemistry reveals marked elevation of alkaline phosphatase (ALP; 911U/L; reference range 20U/L to 150U/L), alanine aminotransferase (336U/L; reference range 10U/L to 118U/L) and total bilirubin (67U/L; reference range 2U/L to 10U/L) indicative of cholestasis. Electrolytes show borderline hypokalaemia (3.6mmol/L; reference range 3.7mmol/L to 5.8mmol/L), most likely as a result of the vomiting. On clinical examination subtle scleral icterus is identified. Abdominal palpation is unremarkable. You decide to perform an abdominal ultrasound (Figures 1 and 2).
Question
What is your interpretation of these images?
Answer

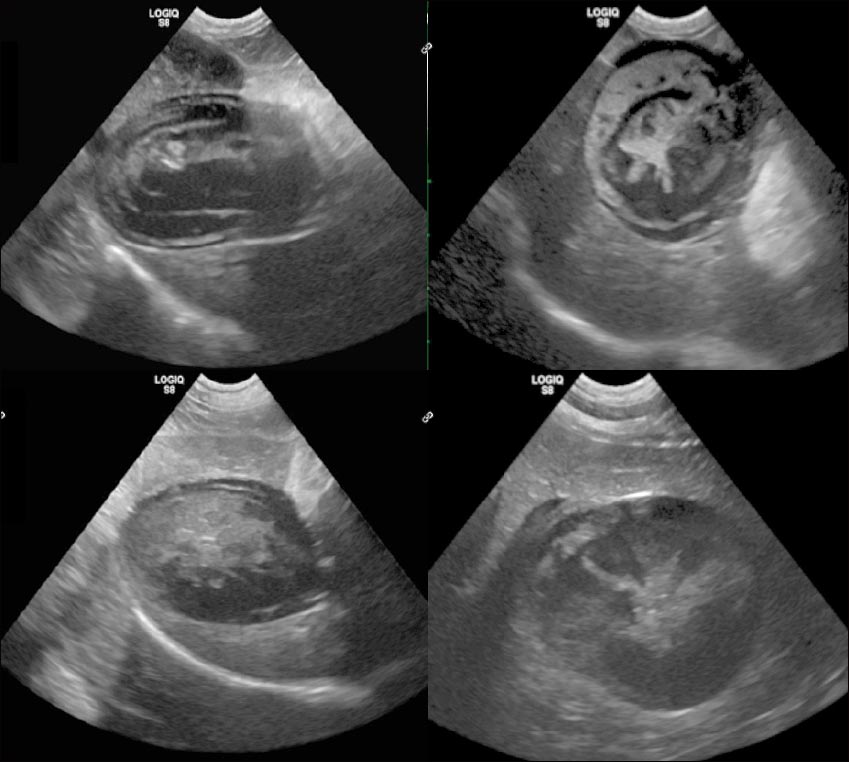
Figure 1 shows a relatively large amount of predominantly centralised echogenic material suspended within the lumen of a distended gall bladder. Several hyperechoic striations radiate peripherally from the centre, creating a stellate appearance, which is sometimes likened to the cut surface of a kiwi fruit. These findings are characteristic of a gall bladder mucocele and, in the author’s experience, older border terriers are highly over-represented.
Figure 2 shows a dilated common bile duct (CBD) surrounded by abnormally hyperechoic fat consistent with localised inflammation. The normal diameter of the CBD in the dog is up to 3mm, whereas Smartie’s CBD measures almost 6mm in diameter and is suggestive of secondary extrahepatic biliary obstruction.
Discussion
Mucoceles represent an abnormal accumulation of intraluminal mucus within the gall bladder that results in progressive gall bladder distension, and, potentially, wall necrosis and rupture. The exact cause is unknown although several contributing factors are likely, including cystic mucinous hyperplasia of the gall bladder wall and gall bladder dysmotility, and animals with dyslipidaemias are predisposed.
Ultrasound is the imaging modality of choice for the diagnosis of a mucocele and they can vary in appearance – depending on their age (Figure 3). Some create a prominent hypoechoic rim between the gall bladder wall and internal organised material, believed to be due to the presence of mucin. Intraluminal material resulting from a mucocele may be differentiated from biliary sludge by the absence of gravity-dependent movement if the patient is repositioned (biliary sludge changes position). The gall bladder wall can also appear thickened and hyperechoic in some patients.
The integrity of the gall bladder wall should be assessed sonographically – any evidence of a discontinuity is consistent with rupture. Ultrasound is reported to have a sensitivity of 94.4% and a specificity of 44.4% for the detection of gall bladder wall rupture, and, in two separate studies, gall bladder rupture occurred in around 50% of dogs with a mucocele. The presence of pericholecystic hyperechoic fat, and/or echogenic peritoneal fluid in the vicinity of the gall bladder, should also raise suspicion of a possible rupture and biliary peritonitis.
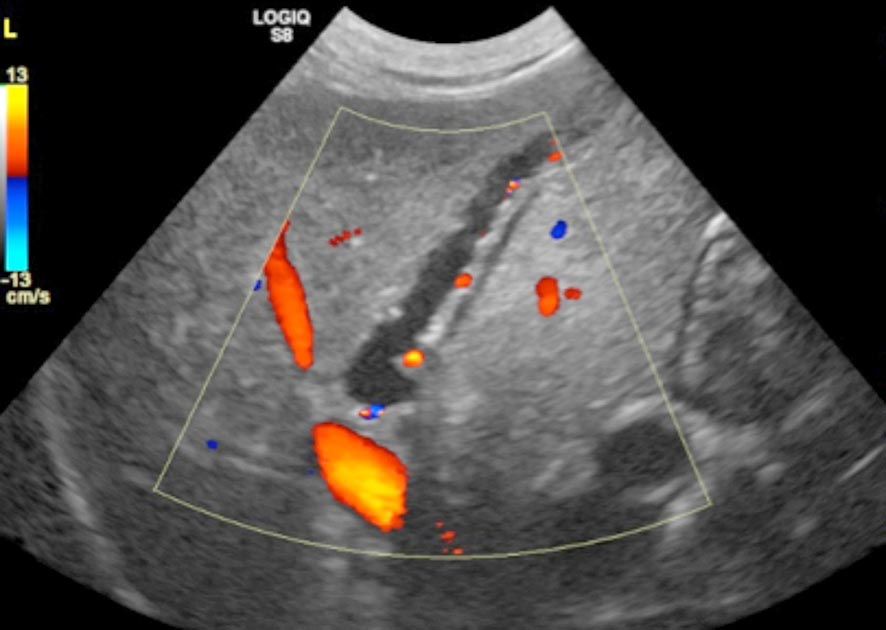
A further potential consequence of a mucocele is the development of extrahepatic biliary obstruction. This can occur if abnormal mucinous material migrates into the CBD, and, in such cases, sonographic evidence of intrahepatic and extrahepatic bile duct dilation may exist. Dilated intrahepatic bile ducts may be recognised on ultrasound by the presence of tortuous vessels with hyperechoic walls and variable diameter travelling through the liver parenchyma. Unlike blood vessels, no evidence will be found of flow within bile ducts when interrogated with colour Doppler. When multiple intrahepatic bile ducts are dilated, this is sometimes referred to as the “too many tubes” sign (Figure 4).
Both surgical exploration – with a view to cholecystectomy or cholecystoduodenostomy – and medical management of gall bladder mucoceles have been reported. In this particular case, Smartie made a full recovery following intraoperative cannulation and flushing of the CBD and cholecystectomy. No evidence was found of gall bladder rupture at surgery.