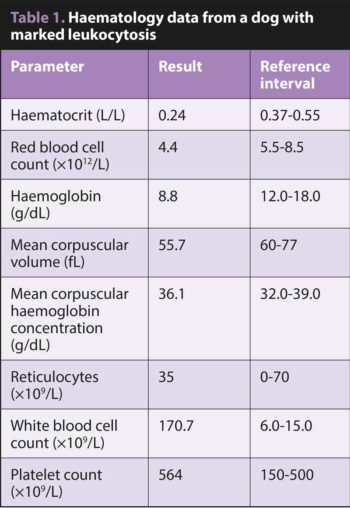
8 Mar 2022
Marked neutrophilia in a dog
Francesco Cian DVM, DipECVCP, FRCPath, MRCVS looks at some of the diagnostics for a case involving a Labrador retriever.

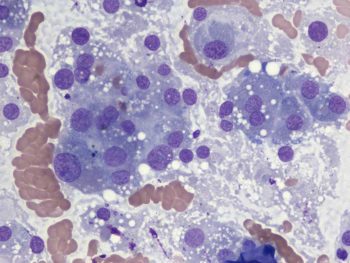
Figure 1. Increased numbers of neutrophils with signs of left shift and mild toxic changes in a dog (peripheral blood, 50x).
The haematology data (Table 1) and the microphotograph (Figure 1) are from an ethylenediamine tetra-acetic acid blood sample of an adult male Labrador retriever seen by the referring veterinarian for a few weeks’ history of reduced general condition, anorexia and episodes of vomiting.
Clinical examination revealed a thin, quiet patient with pale mucous membranes and a strong, regular pulse. Palpation of the abdomen showed a prominent, soft, barrel-shaped liver.
Haematology testing revealed moderate, poorly regenerative anaemia and marked leukocytosis with neutrophilia, signs of toxic changes (increased cytoplasmic basophilia, visible Döhle bodies) and left shift (band neutrophils, metamyelocytes).
Biochemistry analysis showed a marked increase in liver enzymes, total bilirubin and bile acids. On ultrasound examination, a large inhomogeneous liver mass with a diameter up to 8cm was noted.
A fine-needle aspirate of the mass (Figure 2) was collected and submitted for cytological evaluation.
The cytological sample was highly cellular and contained a main population of nucleated cells resembling hepatocytes, but showing marked cytological features of atypia, including anisocytosis (cell size variation), anisokaryosis (nucleus size variation), multinucleation and prominent nucleoli.
What are the main causes of peripheral neutrophilia?
Main disorders that may be associated with marked peripheral neutrophilia in dogs include:
- Focal suppurative processes, including pyometra, pleuritis/pyothorax, peritonitis, prostatitis, pneumonia and/or abscesses. This is the most common differential diagnosis for marked neutrophilia and should be confirmed/ruled out at first.
- Selected infectious disorders including canine babesiosis and canine hepatozoonosis.
- Immune-mediated haemolytic anaemia (IMHA) as it can elicit a systemic inflammatory response.
- Paraneoplastic neutrophilia secondary to underlying malignant neoplasm.
- Chronic neutrophilic leukaemia, a rare myeloproliferative disease mainly diagnosed by exclusion of other causes for neutrophilia.
- Other uncommon causes including leukocyte adhesion deficiency and granulocyte colony-stimulating factor (G-CSF) administration.
Paraneoplastic leukocytosis
In this specific case, paraneoplastic leukocytosis was suspected by exclusion of the other causes (for example, no obvious signs of inflammation, no evidence of IMHA) and most importantly by the concurrent presence of malignancy (hepatocellular carcinoma).
Paraneoplastic leukocytosis has been reported in dogs with several neoplasms in particular carcinomas. It is thought to be caused mainly by overproduction of G-CSF or granulocyte-macrophage colony stimulating factor by neoplastic cells.
What are the most likely causes for this anaemia?
This anaemia is non-regenerative, being microcytic (low mean corpuscular volume) and normochromic (mean corpuscular haemoglobin concentration within reference range) and with low reticulocytes count (less than 70×109/L).
A pre-regenerative condition was ruled out because reticulocytes were persistently low when haematology testing was repeated after four days.
Differentials for truly non-regenerative anaemia include chronic disease/inflammation (too severe in this case to be the only cause), reduced haematopoiesis (for example, chronic renal disease, infectious agents, drug related, liver disease/dysfunction, endocrinopathy), and/or ineffective erythropoiesis (for example nutritional deficiencies, intramedullary IMHA, breed-related dyserythropoiesis).
A combination of chronic disease/inflammation and reduced haematopoiesis due to liver disease were considered likely in this case.